The American Geographical Society's awards ceremony on Wednesday, April 15, at the University of Delaware will honor past and present polar explorers - of this planet and of Mars.
Also recognized will be the researchers who oversaw the gargantuan task of relocating the society's library, described as "the largest privately owned geographical research collection in the western hemisphere," from New York to Wisconsin in the 1970s.
The public is invited to attend the ceremony, which begins at 7:30 p.m. at the Louise and David Roselle Center for the Arts. Register online at this Web page.
The ceremony will be Webcast live at this site and made available as a podcast after the event at the UD podcast Web site.
 | The lecture also will be simulcast into the University of Delaware's virtual world in Second Life, at this location. You must have an avatar in Second Life to visit using this link. Cullum Geographical Medal The Cullum Geographical Medal, "for those who distinguish themselves by geographical discoveries or in the advancement of geographical science, |
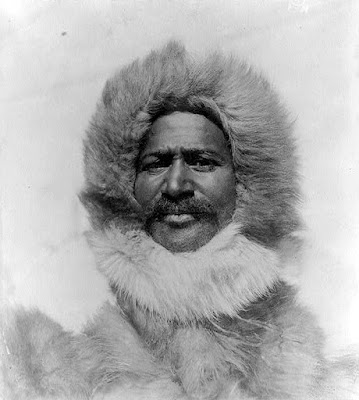
Born in Charles County, Md., Henson became an adventurer early in life, going to sea at the age of 12 as a cabin boy aboard a merchant ship. In 1887, while working as a stock clerk in Washington, D.C., he met Peary, then a U.S. Navy lieutenant, who offered him a job as his valet on a surveying expedition in Nicaragua. Peary was so impressed by Henson's skills and knowledge that he asked him to join him on his arctic adventures over the next two decades, culminating in the 1909 expedition to the North Pole.
Peary repeatedly acknowledged that he could not have reached the top of the world-a feat many believe to have been accomplished on April 6, 1909 - without Henson, who learned all he could from the native Inuit people, including their language, how to build a camp and repair sledges, drive a dog team, make fur clothing, and hunt.
Although Henson's role went largely unacknowledged at the time, later in life he was awarded honorary degrees by Howard University and Morgan College, given lifetime membership in the Explorers Club, and honored at the White House by President Eisenhower. In 1951, he signed the AGS Fliers' and Explorers' Globe at a lavish ceremony in New York's Waldorf Astoria Hotel. Upon his death in 1955, Henson was buried in Woodlawn Cemetery in New York City. In 1988, he was re-interred as a hero, at Arlington National Cemetery alongside Peary.
Leila Savoy Adrade, Henson's great-great grandniece, will accept the Cullum Medal on his behalf. Deirde C. Stam of the Palmer School of Library and Information Science, Long Island University, will offer remarks about Henson's life and accomplishments. In February, Stam republished Henson's 1912 autobiographical account of his North Pole journey. Issued through the Explorers Club of New York, the 2009 edition contains a wealth of new information about Henson.
Peter Smith, senior research scientist at the University of Arizona's Lunar and Planetary Laboratory, led NASA's Phoenix Mars Mission. The Phoenix Mars Lander, the first in NASA's Scout class, was launched on August 4, 2007, and touched down in the Martian arctic on May 25, 2008, to search the soil of the Red Planet for the building blocks of life.
During five months of operations, the probe confirmed the presence of frozen water just below the planet's surface, found minerals that form in liquid water, identified potential nutrients in the soil, and observed snow in the atmosphere. Phoenix's cameras captured more than 25,000 pictures, from grand landscapes to nanoscale images using the first atomic force microscope ever used outside Earth.
Throughout the mission, which ended in November 2008, Smith and his team controlled the lander from the University of Arizona's Science Operations Center, working closely with NASA's Jet Propulsion Laboratory in Pasadena, Calif., and Lockheed Martin Space Systems in Denver. An international assembly of scientific institutes in Canada, Denmark, Finland, Germany, and Switzerland also was involved.
Smith will deliver a public lecture on Thursday, April 16, at 7:30 p.m. at the Center for the Arts. Register for the free event at this Web site.
Samual F. B. Morse Medal
The Samuel Finley Breese Morse Medal, "for the encouragement of geographical research," will be presented to Barbara Borowiecki, professor emerita of geography, and William Roselle, director (retired) of the Golda Meir Library, at the University of Wisconsin-Milwaukee.
Borowiecki made the initial suggestion that the AGS Library in New York be moved to UW-Milwaukee. Used by researchers around the world, the library today numbers more than 1.2 million items, including maps and atlases, books and periodicals, LANDSAT images, photographs, and globes.
She and Roselle prepared a detailed feasibility study that was used to generate support for the project. The pair oversaw many of the details of the library's relocation from uptown Manhattan to Milwaukee, a distance of nearly 1,000 miles. The move took place from July 26 through Sept. 12, 1978, in 16 full-size moving vans.
On Friday, April 17, Roselle will describe "the moving experience" in the Department of Geography's seminar series. The talk will begin at 3:30 p.m. in Room 127 Memorial Hall. A reception will follow.
Borowiecki, a distinguished geomorphologist and horsewoman, was born and raised in Warsaw, Poland. She was a member of the Polish Underground during World War II. Her family immigrated to the United States in the 1940s. After receiving an engineering degree at Indiana University, she enrolled at the University of Wisconsin to pursue her doctorate in geography. Her research and teaching career at UW-Milwaukee focused on eolian and Pleistocene geomorphology and European regional geography.
Roselle, a native of Pennsylvania, received his B.A. from Thiel College and M.L.S. from the University of Pittsburgh. Prior to entering librarianship, he served two years in the U.S. Army and taught at the Milton Hershey School. He held posts at the Pennsylvania State University and the University of Iowa before going to the University of Milwaukee-Wisconsin, where he served two decades as professor and director of the Golda Meir Library. He is the brother of David Roselle, University of Delaware president emeritus.
The award ceremony will include brief remarks by each recipient and be followed by a reception, where Stam and Roselle will sign copies of their books.
Together, the award ceremony and public lecture mark the culmination of the University of Delaware's William S. Carlson International Polar Year Events, celebrating UD's president from 1946-1950, who was an Arctic explorer, and the University's significant polar research in the world's fourth International Polar Year, which began in March 2007 and concluded in April 2009. ###
Contact: Tracey Bryant tbryant@udel.edu 302-831-8185 University of Delaware





































