Study examined physical characteristics as a predictor of obtaining and maintaining leadership roles
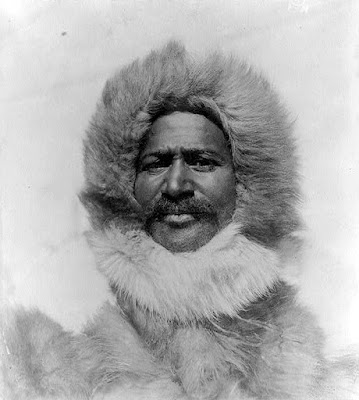
Evanston, Ill. (April 30, 2009) – As President Barack Obama commemorates his 100th day as the country's first black commander-in-chief, a new study by Kellogg School of Management researchers examines the intersection of race and power in corporate America. While many traits of successful leaders transcend racial or ethnic bounds, this study sought to focus on one particular facet of blacks' ascensions to power: the physical characteristics of so-called "babyfaces," and their influence on perception and achievement.
"The Teddy Bear Effect: Does babyfaceness benefit Black CEOs?" will appear in a forthcoming issue of Psychological Science and is co-authored by Robert Livingston and Nicholas Pearce of the Kellogg School.
Methodology
Non-black women and men were shown 40 headshot photos of black men and white women and men. Though the faces were not recognized by participants, all were current or former CEOs of Fortune 500 companies.
The researchers have identified several traits associated with "babyfaceness" including a rounder face, larger forehead, smaller nose, larger ears and fuller, pouty lips. Despite these individual features, babyface is a "gestalt" or whole that is easily recognizable by people. Babyfaceness is an attribute that generalizes across regions, ethnicities, gender and even species, as identified by social psychologists. There is a universal, evolutionary response to babies across all cultures because infants require special care, attention, and nurturing in order to survive.
This adaptive response to infants is over-generalized to adults who have features that resemble babies. The result is that babyfaced adults are treated differently compared with maturefaced adults: babyfaced adults are considered more warm, innocent and trustworthy.
The hypothesis of the current study was that babyfaceness could serve as a "disarming mechanism" that would attenuate the fear, hostility and aggression typically associated with black males. Thus babyfaceness would facilitate the ascension of black males but not white males.
Results
Babyface features had a clear influence on professional achievement, both perceived and real. Black CEOs were rated as being more babyfaced, and having warmer personalities, than whites.
The more babyfaced the black CEO, the more he was also thought to earn. In terms of real, not just perceived, earnings and achievement, the more babyfaced the black CEO, the more prestigious was the company he actually led, reflected by both Fortune 500 ranking and annual corporate revenue. These perceived and real professional benefits were correlated with physical appearance, not to perceptions of age, which was not found to be linked to babyfaceness.
Livingston pointed out that while the 10 black CEO faces were considered warmer than the white faces, blacks as a group were considered less warm than whites overall. Thus, the visual influence of babyfaceness clearly shifted perception, and the playing field. He said, "To function effectively as an African American male in the U.S. it helps to have a disarming mechanism." A disarming mechanism is a physical or behavioral trait, noted Livingston, that eases perceptions of threat—it signals to whites that they do not have a reason to fear this particular black individual. Babyfaceness is but one example: political conservatism, style of speech or dress, smiling behavior, or even a Harvard education might also serve a similar disarming function.
The research notes disarming mechanisms, like warmth, are only necessary for groups that are perceived to be hostile or threatening by default. Prior research has shown warmth to be counterproductive for white male leaders and women leaders. "Female leaders are already 'disarmed' because of traditional caregiver roles and stereotypes," said Livingston. "Women leaders must prove to be strong and assertive, frequently at the expensive of being perceived as lacking warmth." The implication is that black leaders may have to adopt a gentler leadership style compared with white males who can get angry or pound their fists in order to accomplish leadership objectives.
Beyond the Babyface
While facial features may present natural advantages or obstacles to some, other behavioral traits can be developed and used by most anyone. "There are other mechanisms thought to help minorities function and achieve without stoking envy, resentment, fear," said Livingston. "For example, some point to Former U.S. Secretary of State Condoleeza Rice as someone who internalizes shared ideology with the dominant group, and is therefore seen as non-threatening." Livingston adds that although Barack Obama does not possess all of the typical features associated with babyfaceness per se, he does have a disarming appearance. "Big ears or a simple smile can disarm one's appearance from suggested perceptions of threat that might otherwise be associated with black males. This could serve to increase the appeal of the president or even one of Hollywood's most successful actors—Will Smith," he said. ###
- To read the full article or speak with Kellogg School of Management professor Robert Livingston, e-mail Meg Washburn at m-washburn@kellogg.northwestern.edu
- To learn more about the Association of Psychological Science, visit www.psychologicalscience.org.
- To learn more about the Kellogg School of Management, visit www.kellogg.northwestern.edu.