Gene expression pattern of the MYH9 gene.
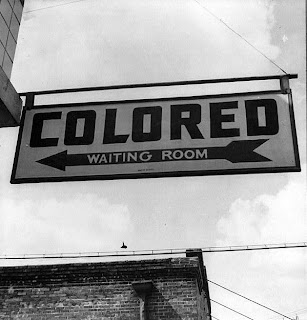
Possible new approaches to screening and prevention in African-American families
Several recent studies have suggested that common gene variations may be responsible for much of the elevated risk of kidney disease in African Americans. New research on the MYH9 gene—and its implications for the screening and possible prevention of kidney disease in the African American population—will be summarized in a press briefing to be held at the American Society of Nephrology's 41st Annual Meeting and Scientific Exposition in Philadelphia, PA.
"The susceptible variants in the gene MYH9 are very frequent among African Americans and account for a substantial proportion of the higher risk of end-stage renal disease (ESRD) in African Americans compared to European Americans," comments Rulan S. Parekh, MD, of Johns Hopkins University School of Medicine in Baltimore, MD, who will introduce the press briefing. "Discovery of this gene has opened up a new area of research to focus on both the mechanism of disease and also potential use for screening in the population."
In September, researchers from the National Institutes of Health (NIH) in Bethesda, MD, and Johns Hopkins University published independent studies showing that variations of the "non-muscle myosin heavy chain 9" gene (MYH9) are linked to certain types of kidney disease that are more common in African Americans, including focal segmental glomerulosclerosis (FSGS), HIV-associated nephropathy, and non-diabetic ESRD.
Variations of MYH9 may also explain the increased rate of hypertension-related kidney disease in African Americans, which tends to persist even with effective treatment to lower blood pressure. Overall, the gene variants appear to increase the risk of developing any form of ESRD, which is irreversible kidney failure requiring dialysis or transplantation not related to diabetes.
The discoveries have major public health implications because of the high frequency of MYH9 variants among African Americans with kidney disease: up to 60 percent, compared with four percent of European Americans.
At the press briefing, Dr. Parekh will introduce a panel of researchers at the forefront of ongoing research on MYH9. The speakers will share their perspectives on the discoveries so far, key areas for further study, and the implications for risk screening and efforts to reduce kidney disease in the African-American population.
Cheryl Winkler, PhD, of NIH will summarize key findings on the link between MYH9 and FSGS, including the methods and concepts that led to the discoveries. New studies by Dr. Winkler, along with Jeffrey Kopp, MD, and other NIH researchers, suggest that MYH9 explains most of the racial difference in FSGS risk (F-FC254). Research by Dr. Kopp and Dr. Winkler will also be presented as part of a free communications session entitled, "Gene Mapping in Common Kidney Diseases" on Friday, November 7, from 4:00 p.m.-6:00 p.m. in Room 104 of the Pennsylvania Convention Center.
Dr. Winkler will also discuss new research on the geographic distribution of the MYH9 risk alleles (TH-PO107). Rates of highest-risk gene variant appear highest in populations from southern Africa; in contrast, the high-risk allele is infrequent in Europeans, and "rare to absent" in Asians. The findings suggest that selection of the high-risk MYH9 risk variants was an ancient event in human evolution (TH-PO109). Dr. Winkler will also present her research findings for poster numbers TH-PO107 and TH-PO109 on Thursday, November 6, from 10:00 a.m.-Noon in Hall A/B of the Pennsylvania Convention Center.
Linda Kao, PhD, of Johns Hopkins University will focus on the risk of non-diabetes-related ESRD related to MYH9 variants. Dr. Kao and Dr. Parekh were involved in the genome-wide study showing that the risk of nondiabetic ESRD is strongly related to higher African American ancestry on chromosome 22 (F-FC255). People with the MYH9 at-risk variants were at up to double the risk of having nondiabetic ESRD. In contrast, MYH9 does not affect the risk of ESRD resulting from diabetes, which remains the most common cause of kidney disease. Dr. Kao's research will also be presented as part of a free communications session entitled, "Gene Mapping in Common Kidney Diseases" on Friday, November 7, from 4:00 p.m.-6:00 p.m. in Room 104 of the Pennsylvania Convention Center.
Barry I. Freedman, MD, of Wake Forest University in Winston-Salem, NC, will discuss evidence on the relationship between MYH9 and early kidney disease. A new study suggests that these common MYH9 variants are related to albuminuria—leakage of the protein albumin in the urine, an early sign of kidney disease—in African Americans with high blood pressure, but not necessarily in European Americans (TH-PO108). Many cases of kidney disease attributed to hypertension or unknown causes in African Americans may actually be related to MYH9 variants, through a process similar to FSGS (TH-PO94). It's too early to tell whether MYH9 is related to lupus nephritis—another cause of kidney disease that's more common in African Americans (TH-PO106). On Thursday November 6, Dr. Freedman will also present his research on poster numbers TH-PO108, TH-PO94, and TH-PO106 from 10:00 a.m.-Noon in Hall A/B of the Pennsylvania Convention Center.
Dr Kopp will summarize the findings of the genetic risk associated with MYH9 variants and kidney disease. He will also address the implications of the new discoveries for patients and physicians, including the possible role of MYH9 screening.
The presentations will be followed by a brief question-and-answer session, moderated by Dr. Parekh. It's important to note that most African Americans with MYH9 gene variants will not develop kidney disease. However, MYH9 gene testing may become an important new tool to identify African American patients and families at increased risk. "In the future, therapeutics and screening may target those who have MYH9 genetic variants to prevent progression to ESRD," according to Dr. Parekh. ###
The Press Briefing, "Discovery of a Gene Associated with Kidney Diseases among African Americans," will be presented on Friday, November 7, 2008, from 12:15 p.m.-1:15 p.m. in Room 303A of the Pennsylvania Convention Center in Philadelphia, PA.
ASN is a not-for-profit organization of 11,000 physicians and scientists dedicated to the study of nephrology and committed to providing a forum for the promulgation of information regarding the latest research and clinical findings on kidney disease. ASN Renal Week 2008, the largest nephrology meeting of its kind, will provide a forum for 11,000 nephrologists to discuss the latest findings in renal research and engage in educational sessions related to advances in the care of patients with kidney and related disorders. Renal Week 2008 will take place November 4 – November 9 at the Pennsylvania Convention Center in Philadelphia, PA.
Contact: Shari Leventhal
sleventhal@asn-online.org WEB:
American Society of NephrologyImage Licensing: Permission is granted to copy, distribute and/or modify this document under the terms of the
GNU Free Documentation License, Version 1.2 or any later version published by the Free Software Foundation; with no Invariant Sections, no Front-Cover Texts, and no Back-Cover Texts.
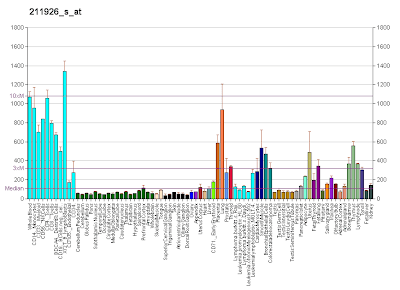
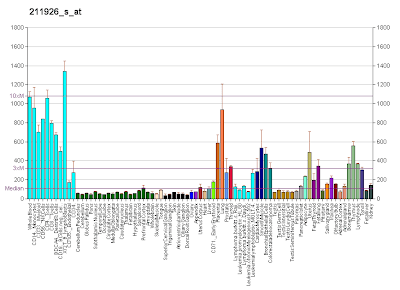
* Image Description: Gene expression pattern of the MYH9 gene.
* Image Source: Diagram created by User:AndrewGNF based on data from Su AI, Wiltshire T, Batalov S, et al (2004). "A gene atlas of the mouse and human protein-encoding transcriptomes". Proc. Natl. Acad. Sci. U.S.A. 101 (16): 6062–7. doi:10.1073/pnas.0400782101. PMID 15075390. Creation supported by the Genomics Institute of the Novartis Research Foundation.