Wednesday, November 26, 2008
Research demonstrates differing genetic makeup of lung cancer in African-American patients
Previous studies have determined that ethnicity can have an influence on the risk and outcome of non-small cell lung cancer patients, with African-American patients experiencing a higher risk and poorer outcomes. Ethnic background can also impact the genetic make-up and responsiveness of non-small cell lung cancer to EGFR gene blocking drugs. For example, a large number of Asian patients carry mutations of the EGFR gene than Caucasians, which can determine the likelihood of major clinical responses to EGFR inhibitor drugs while a higher copy number of EGFR is a predictor of better long-term outcome with the use of these drugs.
Researchers at the Departments of Medicine, Pathology and Biostatistics at Case Western Reserve University in Cleveland; the Departments of Medicine and Pathology at the University of Colorado Cancer Center in Aurora, Colo.; and the Instituto Clinico Humanitas IRCCS in Rozzano, Italy, sought to determine the frequency of EGFR abnormalities in African American patients since there is a paucity of data on this population.
The study authors observed 53 African-American patients with resected non-small cell lung cancer and found few EGFR mutations and an increase in the frequency of tumors with a high copy number of the EGFR gene. Previous studies have shown that an increase in the number of copies, regardless of mutation, predicts a better outcome with EGFR inhibitor drugs.
"The findings of this study were surprising since it was not expected that drug-sensitizing EGFR mutations would be so rare in this patient population," Rom Leidner, M.D., one of the study's authors and a clinical fellow in hematology/oncology at Case Western Reserve University said. "African-American patients remain underrepresented in clinical studies in oncology and therefore our knowledge base about how to modify our treatment strategies for this patient population remains poorly defined."
Researchers hope that the findings of their study could impact how clinical studies are designed in the future and how EGFR-targeted agents are used in the future. ###
The abstract, "A Study of Genetic Abnormalities of the EGFR Pathway in African American Patients with Non-Small Cell Lung Cancer," will be presented in a poster discussion session Friday, November 14, 2008 from 9:30 a.m. to 10:00 a.m. To speak to Dr. Leidner, please call Beth Bukata or Nicole Napoli on November 13-14, 2008, in the Press Room at the Chicago Marriott at 312-595-3177. You may also e-mail them at bethb@astro.org or nicolen@astro.org.
Contact: Beth Bukata bethb@astro.org 703-839-7332 American Society for Therapeutic Radiology and Oncology
Image Licensing: I, (Boghog) the copyright holder of this work, hereby release it into the public domain. This applies worldwide.
In case this is not legally possible: (Boghog) I grant anyone the right to use this work for any purpose, without any conditions, unless such conditions are required by law.
Monday, November 24, 2008
Hypertension develops early, silently, in African-American men
Kevin Heffernan, Ph.D. ostdoctoral Fellow Molecular Cardiology Research Center Tufts Medical Center 800 Washington Street, Box 080 Boston, MA 02111, 617-636-1441 Kevin Heffernan Kevin Heffernan was born and raised in the Bronx NY. He completed his BS in Exercise Science at the University of Scranton, his MS in Applied Physiology and Nutrition at Columbia University, and his PhD in Kinesiology/Exercise Physiology at the University of Illinois at Urbana-Champaign. Kevin has recently joined the Vascular Function Study Group in the Division of Cardiology. His research will focus on novel mechanisms influencing endothelial function and exercise capacity in patients with cardiovascular disease. When Kevin is not in the lab he enjoys resistance training, long walks on the beach and candlelit dinners. | Study points to central blood pressure as key to screening BETHESDA, Md. (Nov. 17, 2008) − Young and healthy African-American men have higher central blood pressure and their blood vessels are stiffer compared to their white counterparts, signs that the African American men are developing hypertension early and with little outward sign, according to a new study. While the study found that central blood pressure -- the pressure in the aorta, near the heart -- was higher in the African-American men, the study found no difference in brachial blood pressure -- measured on the arm -- between the two groups. Taken together, the findings suggest that hypertension (high blood pressure) may be developing undetected in young African-American men and that measuring central blood pressure may be a better means of detecting the problem as it develops. "Central blood pressure holds greater prognostic value than conventional brachial blood pressure as central pressure more aptly reflects the load encountered by the heart," the authors explained. "Thus, brachial blood pressure may neglect important information on cardiovascular burden and response to therapy in African-American men." |
'Silent killer'
African-American men have higher levels of hypertension than white men. Hypertension is known as the silent killer because it can develop without the individual knowing it. According to the U.S. Centers for Disease Control and Prevention, hypertension is a major risk factor for heart disease, stroke, congestive heart failure, and kidney disease. In 2002, hypertension was listed as a primary or contributing cause of death for 277,000 Americans.
The University of Illinois researchers hypothesized that the blood vessels of the black men would show greater dysfunction than the white men, even though both groups were young and equally healthy and fit. The vascular damage they looked for included stiffening and thickening of the blood vessels. These conditions result in pulsatile (not smooth) blood flow (and at higher pressure) to organs. The pressure can damage the organs over time.
Both groups healthy
The study included 55 young men, 30 white and 25 African-American. Most were university seniors. The average age was 23. There were no differences between the groups on a variety of measures, including heart rate, cardiorespiratory fitness, body mass index, body fat, blood lipids and glucose levels.
The researchers measured vascular function in a variety of ways, including:
* aortic blood pressure and stiffness
* brachial blood pressure
* carotid artery blood pressure
* carotid artery thickness and stiffness
They found the African-American men had similar brachial blood pressure, compared to the white men, but they had significantly higher:
* Central blood pressure, a measure of the pressure found in the artery, near the heart. The researchers used an instrument that takes blood pressure at the wrist and then calculates the central blood pressure.
* Carotid artery pressure. The carotid artery runs through the neck.
The African-American men, unlike the white men, also showed signs of early vascular damage that could lead to hypertension. For example, they had:
* Thicker carotid arteries, a sign of vascular damage that is usually found in older individuals and associated with atherosclerosis.
* Stiffer arteries, which are associated with high blood pressure. When the heart beats, blood flows through stiff arteries at greater speed and pressure. Elastic arteries provide a smoother blood flow and help prevent damage to organs receiving the blood and place less stress on the heart.
* Less change in diameter of the arteries when the heart beats, another measure of vascular stiffness. A healthy artery is more elastic will change in size as the blood flows through with each beat of the heart.
"Although having a similar cardiovascular risk factor profile as young white men, diffuse macrovascular and microvascular dysfunction is present at a young age in apparently healthy African American men," the authors wrote. "Values seen are comparable to values often reported in older individuals or individuals with more advanced hypertensive disease," they said.
These results do not shed light on why this happens to young and fit African-American men, Heffernan said. There may be environmental differences, such as differences in diet, which were not examined as part of this study, he said. ###
Editor's Notes: To arrange an interview with Dr. Heffernan, please contact Christine Guilfoy at cguilfoy@the-aps.org or (301) 634-7253.
A fuller audio interview with Dr. Heffernan is available in Episode 15 of the APS podcast, Life Lines, at www.lifelines.tv.
Funding: American Heart Association and the American College of Sports Medicine
Physiology is the study of how molecules, cells, tissues and organs function to create health or disease. The American Physiological Society (APS) has been an integral part of this scientific discovery process since it was established in 1887.
Find the full interview with Dr. Kevin Heffernan in Episode 15 of Life Lines. Interview begins at 13:26. The link is at lifelines.libsyn.com/
Contact: Christine Guilfoy cguilfoy@the-aps.org 301-634-7253 American Physiological Society
Saturday, November 22, 2008
African-Americans with depression and heart attack have greater risk of death
Using the Patient Health Questionnaire as part of a prospective myocardial infraction registry, Parashar and her team measured depressive symptoms in 397 African-American MI patients at Grady Memorial Hospital in metro Atlanta.
Patients were assessed and categorized as past, new, persistent or never depressed. Patients were followed up for a maximum of 58 months after MI. Researchers examined the relative prognostic importance of current, past versus persistent depression on mortality among African Americans with acute MI adjusting for demographic, clinical and quality of care variables.
Preliminary results show patients with persistent depression were almost three times as likely to die after MI compared with never depressed patients. ###
Contact: Juliette Merchant jmmerch@emory.edu 404-778-1503 Emory University
Thursday, November 20, 2008
Black entrepreneurs 4 times more likely to be refused credit than white businesses
 Stuart Fraser, Associate Professor of Enterprise Centre for Small and Medium Sized Enterprises, Enterprise Group. Room D1.18 (Social Studies Building) Warwick Business School The University of Warwick Coventry, CV4 7AL, UK. | A research paper, by Dr Stuart Fraser of Warwick Business School at the University of Warwick, has found that many Ethnic Minority owned Businesses (EMBs) in the UK struggle to obtain credit in comparison to White owned businesses. Black and Bangladeshi owned businesses are the most likely to be refused credit, facing up to four times as many refusals as white owned businesses. Warwick Business School researcher Dr Stuart Fraser examined the small business credit market using data from the UK Survey of Small and Medium Finances (UKSMEF). He found that in particular Bangladeshi and Black owned firms are several times more likely to be denied loans than Indian and White owned businesses. The survey found that 36% of Black African firms had been denied loans compared to 29% of Black Caribbean, 20.6% of Bangladeshi, 12.2% Pakistani, 7.3% Indian, and 8.2% white owned businesses. |
The research found that one clear reason for this much higher incidence of missed loan repayments and exceeding overdraft limits (financial delinquency) was the much younger age of the Pakistani, Bangladeshi and Black owned firms compared to Indian and White firms. Black African owned businesses averaged 6 years, Black Caribbean 6.9, Bangladeshi, 6.5, Pakistani 8.3, Indian 14.2, and White owned 18.7 years. Other key reasons for financial delinquency include the business owner lacking a financial qualification or suitable financial advice and the business already having too much debt. In the case of Black African firms the research also points to cultural differences as a possible explanation for higher delinquency rates.
The research also found that Black Caribbean firms in the UK are less likely to apply for loans than White owned businesses due to fears of rejection based upon discrimination.
Dr Fraser points to the increasing use of 'arms length' credit and behavioural scoring systems, which do not allow transactions to be tainted by dubious judgements based upon ethnic perceptions by loan officers. He notes that scoring systems may explain the absence of racial bias, but ironically, they may also be responsible for misperceptions of racial bias since the reasons for rejection are not usually made clear to the applicant in these cases.
Dr Fraser says "Improvement in information flows between finance providers and businesses about the criteria used to make credit assessments including providing the reasons for rejection would help tackle the misperceptions of discrimination. In particular, finance providers should make it more clear to EMBs that defaulting on a loan or exceeding an overdraft limit could have adverse consequences for future credit."
This research highlights a number of factors which need to be addressed in order to reduce ethnic variations in loan denial rates: lack of financial skills and advice; poor financial performance; and ethnic and cultural differences. Targeting EMBs for assistance with skills advice may help reduce delinquency rates and improve access to finance. This, together with finance providers investing more in their relationships with Black firms could cause significant reductions in dissatisfaction. ###
Download the research paper: Is there Ethnic Discrimination in the UK Market for Small Business Credit?
For further information please contact: Peter Dunn, Press and Media Relations , University of Warwick Tel: +44 (0)24 76 523708 cell/mobile +44 (0)7767 655860 p.j.dunn@warwick.ac.uk Or Vincent Hammersley, Director of Communications
Warwick Business School Tel +44 (0) 2476 524124 Cell/Mobile +44 (0)7985 956624 Vin.Hammersley@wbs.ac.uk
Tuesday, November 18, 2008
Fear, misconceptions about screenings keep many African-Americans from getting mammograms
The findings are based on feedback gathered during focus groups that included 29 low-income African-American women who were at least 40 years old. The women were asked about their perception of mammograms, whether they would undergo one to screen for breast cancer, and other related questions.
Despite recommendations for women 40 and older to have annual mammograms, only 55 percent of the women reported having a mammogram within the last two years. One woman in the study had a history of breast cancer.
Participants in the study were low-income, medically underserved African-American women who lived in urban, economically challenged neighborhoods throughout Chicago. Participants received a $15 gift certificate to a grocery store in exchange for their participation.
Asked why they did not go for regular mammograms, women in the study gave several reasons. Some felt they had not been treated with respect or not received adequate information from clinical teams during prior visits to health care facilities.
One woman recounted feeling uncomfortable when she was left alone while her images were being developed and read by a radiologist.
"You see, when they left me, there wasn't nobody with me to talk to me," she said.
Other study participants said they thought anyone with breast cancer would inevitably die from the disease, so there was no use getting a mammogram.
"I didn't know that it was a possibility to live after you had breast cancer or had been found having breast cancer," one woman said.
"Everybody I know who had breast cancer [has] died. I [wasn't aware] of anything different," another woman said.
Women also said that stories circulate of patients who had bad experiences undergoing mammograms and received incorrect cancer treatments, such as an unnecessary mastectomy. Those tales are all spun into the urban folklore about mammograms and impact women's decisions not to get screened. The study adds that because of their fears, some women delay getting screened, which leads to worse health outcomes such as late-stage cancer diagnosis and higher mortality rates.
The study points to the need for physicians to be trained in cultural sensitivity. If health care providers tailored their care appropriately for this population, these patients may be more likely to return for repeat mammograms. The study also suggests the need for more community-based health educators to work within underserved communities, explaining the breast cancer screening process, addressing misperceptions, and reinforcing the health messages women receive from their physicians.
"African-American women have a high need for comprehensive information and better communication from their health care providers on breast cancer prevention and treatment. Sadly, we heard none of the women in our study were aware of early diagnosis or positive breast cancer outcomes," Peek said. ###
The study was funded by the Open Society Institute's Medicine as a Profession (MAP) fellowship program and Susan G. Komen for the Cure. Peek is currently supported by the Robert Wood Johnson Foundation Harold Amos Medical Faculty Development program.
Additional study authors include Judith Sayad and Ronald Markwardt.
Contact: Martha O'Connell Martha.OConnell@uchospitals.edu 773-834-8089
University of Chicago Medical Center
Sunday, November 16, 2008
Efforts for whites to appear colorblind may backfire
Tufts University researchers find that efforts to avoid the topic of race may have unintended results
MEDFORD/SOMERVILLE, Mass. -- New research shows that whites often avoid using race to describe other people, particularly in interactions with blacks. However further research reveals that such efforts to appear colorblind and unprejudiced are associated with less-friendly nonverbal behaviors.
"Many whites seem to think that appearing colorblind – avoiding race during social interaction – is a good way to appear unbiased," said Samuel R. Sommers, Ph.D., assistant professor of psychology in the School of Arts and Sciences at Tufts University. "Despite that perception that colorblindness may make a positive impression on others, our data suggests that it often backfires."
Claiming color blindness
In the first study, 57 white participants completed either a "sorting task" or a "hypothetical task." With the sorting task, participants sorted 24 photos of black and white volunteers according to seven characteristics: race, gender, age, color of the background in the photo, hair color, facial expression, and facial hair. In the hypothetical task, participants were asked to estimate how quickly they would categorize using each of the seven characteristics if they were to perform the sorting task.
The results for the sorting task showed that participants were quickest to categorize the photos by background color, then gender, then race. However, in the hypothetical task, participants estimated that the two slowest characteristics to determine would be race followed by age. Further research showed that blacks' speed at categorizing photos by race was comparable to whites' but their estimates of their ability to do this were more accurate than the estimates of white participants.
"Whites sometimes deny the ease with which they can categorize others by race," Sommers said. "And they'll even avoid using race as a simple descriptor of someone else."
Political correctness has surprising results
The second study examined some of the possible consequences of whites' reluctance to use race to differentiate people. Thirty white participants were randomly paired with a white or black partner who was in fact a "confederate" in the research project. The pair played a game in which one person asked questions to identify a target face in a set of photos. Questioners were told that their objective was to identify the photo the answerer was looking at by asking as few yes/no questions as possible.
The white participants, who all played the role of questioner, were given 32 photos of faces that varied by the same categories as those in the first study, including gender, background color and race. The "confederates" acted as answerers and were given a copy of the target photo. They answered yes or no questions until the questioner determined which of the 32 photos the answerer held.
The results showed that the questioner was less likely to mention race when the answerer was black (64 percent of the time) than when the answerer was white (93 percent of the time). This led to less-efficient performance times when white questioners were paired with black answerers because they asked more questions to identify the target photo.
In addition to slower performance, reluctance to differentiate by race was associated with less friendly nonverbal behaviors.
"When we showed independent coders video clips of questioners in the study without audio, they noted that the white participants who avoided talking about race with a black partner made less eye contact with their partners and appeared to be less friendly," Sommers said. "By their nonverbal behavior alone, the whites who are trying to appear colorblind to impress their black partners ironically come across as distant and unfriendly." ###
CONTACT: Kimberly M. Thurler kim.thurler@tufts.edu (617) 627-3175
Tufts University, located on three Massachusetts campuses in Boston, Medford, Somerville, and Grafton, and in Talloires, France, is recognized among the premier research universities in the United States. Tufts enjoys a global reputation for academic excellence and for the preparation of students as leaders in a wide range of professions. A growing number of innovative teaching and research initiatives span all Tufts campuses, and collaboration among the faculty and students in the undergraduate, graduate and professional programs across the university's eight schools is widely encouraged.
Contact: Suzanne Miller suzanne_c.miller@tufts.edu 617-627-4703 Tufts University
Friday, November 14, 2008
Gifts, affirmations boost medication adherence in African-Americans
 PDF of Image | A patient education program that included self-affirmation and positive affect in the form of occasional gifts significantly increased medication adherence among African Americans with high blood pressure, according to research presented at the American Heart Association's Scientific Sessions 2008. The randomized, controlled trial found that calling patients occasionally with positive messages, coupled with standard information about hypertension encouraged them to take their medication more often than patients who received usual care. |
Adherence — taking medication consistently and correctly — is a major issue in all patient populations and especially African Americans.
"African Americans have been shown in some studies to be nearly twice as likely to not take their medicines when compared to Caucasians," Ogedegbe said.
For this study, researchers measured adherence, with electronic monitors installed on the caps of the blood pressure pill bottles. The monitors recorded each time the pill bottles were opened. Researchers consider this method far more reliable than patient self-report.
The study of 252 African Americans with hypertension found that those who received unexpected quarterly gifts by mail plus bi-monthly calls reminding them of positive life experiences took their medication 43 percent of the time over 12 months. Patients who just received a workbook on their disease with no additional intervention (control group) took their medicines 36 percent of the time during the year-long study.
"The adherence level is still woefully low," Ogedegbe said.
Of the study patients, 80 percent were women, average age 58. All were prescribed at least one anti-hypertension medication.
Although, most of the study participants were women, Ogedegbe expects the results to also apply to African-American men.
Each patient in the study in the intervention group and in the control group received a 10-chapter hypertension education workbook that detailed ways to combat hypertension. Those in the intervention group also were called every two months with homework from the workbook along with reminders to think about proud moments in their lives, their goals and the values they hold dear. The calls were not costly, Ogedegbe said, because they came from research assistants with college degrees rather than medical professionals.
The intervention group also received up to six small gifts unexpectedly throughout the 12-month study duration, which included an umbrella and a duffle bag. The items were adorned with positive messages such as, "It's a beautiful day."
"The whole idea is to reduce the amount of negativity patients have in terms of their health," Ogedegbe said. "If you are depressed, you are much less likely to take your medicine. This study attacked it from two ways by reducing the rate of depressed feelings and helping patients affirm their own positive feelings. When people receive unexpected good news or gifts it tends to induce positive feelings and it is shown to carry over into other areas of life." ###
Co-authors are: Carla Boutin-Foster, M.D; Martin T. Wells, Ph.D.; John P. Allegrante, Ph.D.; Jared B. Jobe, Ph.D.; and Mary E. Charlson, M.D.
Individual author disclosures can be found on the abstract.
The National Heart Lung and Blood Institute funded the study.
Statements and conclusions of study authors that are presented at American Heart Association scientific meetings are solely those of the study authors and do not necessarily reflect association policy or position. The association makes no representation or warranty as to their accuracy or reliability. The association receives funding primarily from individuals; foundations and corporations (including pharmaceutical, device manufacturers and other companies) also make donations and fund specific association programs and events. The association has strict policies to prevent these relationships from influencing science content. Revenues from pharmaceutical and device corporations are available at www.americanheart.org/corporatefunding.
Contact: AHA News Media Staff Office bridgette.mcneill@heart.org 504-670-6524 American Heart Association
Wednesday, November 12, 2008
Blood Pressure Control Inequality Linked to Deaths Among Blacks
Kevin Fiscella, M.D., M.P.H. Associate Professor of Family Medicine and Community & Preventive Medicine with tenure, University of Rochester School of Medicine & Dentistry Associate Director, Rochester Center to Improve Communication in Health Care HIV Clinical Coordinator, Westside Community Health Center | Racial disparity in the control of hypertension contributes to the deaths of almost 8,000 black men and women in the United States annually, according to a first-of-its-kind study published today in the Annals of Family Medicine by University of Rochester Medical Center researchers. The researchers concluded that the deaths could be avoided or postponed if blacks had their hypertension, or high blood pressure, controlled to the same level as whites. “Disparity in the control of blood pressure is one of the most important, if not the most important, contributor to racial disparity in cardiovascular mortality, and probably overall mortality,” said Kevin Fiscella, M.D., M.P.H., lead author of the article and associate professor of family medicine and of community and preventive medicine at the Medical Center. “If we as clinicians are going to reduce cardiovascular and stroke-related deaths, we need to pay attention to all the barriers to improving blood pressure control, particularly for minority patients” Fiscella said. Although not clearly known, the likely causes of the racial disparity include differences in access to care, clinician management and communication, hypertension severity, and patient adherence. |
“There is evidence from previous studies that access barriers and financial and interpersonal communication barriers affect the ability of black patients to get medical care or to take their medication as prescribed,” Fiscella said.
Fiscella and Kathleen Holt, Ph.D., adjunct professor of community and preventive medicine at the Medical Center, are authors of the articles, which is the first effort to quantify the toll of racial disparity in blood pressure control. The article is part of a package of articles on racial disparity in the Annals of Family Medicine that is accompanied by editorials from former U.S. Surgeon General David Satcher, M.D., Ph.D., and Crystal Wile Cené, M.D., M.P.H., and Lisa A. Cooper, M.D., M.P.H. They call on clinicians, researchers, health care administrators, health care planners and policy makers to work together to gain a better understanding of the barriers faced by ethnic minorities.
Hypertension is a precursor to cardiovascular disease, which is the leading cause of death in the United States and which occurs at the highest rate among black Americans.
The researchers analyzed data of 1,545 black adults and 1,335 white adults. The mean blood pressure among blacks with hypertension was approximately six mm/Hg (millimeters of mercury) higher than that for the total adult black population and seven mm/Hg higher than that for whites with hypertension.
A reduction in mean blood pressure among blacks to that of whites would reduce the annual number of deaths among blacks from heart disease by 5,480 and from stroke by 2,190, the researchers concluded.
“There is evidence for racial disparity in patient adherence to antihypertensive medication, including studies conducted within the Veterans Administration Health System, where fewer differences in access appear to exist,” the researchers state in the article. “Differences in adherence by race may be due to affordability of medicines, personal beliefs, anticipated adverse effects, and health literacy that disproportionately affect blacks. Although multiple causes may contribute to racial disparity in blood pressure control, this disparity is not inevitable. Disparity in hypertension control is significantly smaller in the Veterans Administration Health System, where access barriers are fewer.”
Elimination of racial disparity in blood pressure control is an attainable goal, provided sufficient resources are available to discover and address adherence barriers, the researchers conclude.
Funding for the research was provided by the Robert Wood Johnson Foundation and through a grant from the National Heart, Lung, and Blood Institute.
Contact: Michael Wentzel Michael_Wentzel@urmc.rochester.edu 585-275-1309 University of Rochester Medical Center
Monday, November 10, 2008
ERSD, heart disease and African-Americans with hypertensive nephrosclerosis
For most patients with chronic kidney disease (CKD), the risk of experiencing a cardiovascular related death is greater than the risk of progressing to end-stage renal disease (ESRD).
According to research being presented at the American Society of Nephrology's 41st Annual Meeting and Scientific Exposition in Philadelphia, Pennsylvania, African Americans with CKD caused by high blood pressure (hypertensive nephrosclerosis) demonstrated a higher risk of progressing to ESRD than dying from heart disease related events.
Tahira Alves, MD, of Vanderbilt University in Nashville, Tennessee, will present the cardiovascular and renal results from the AASK (African American Study of Kidney Disease) Cohort Study (2002-2007), which followed the original AASK Trial (1996-2001).
The risk of death from cardiovascular disease was 0.8 per 100 patient-years. Of 74 deaths that occurred during the Cohort period of the AASK Study, more than 60 percent were from causes other than cardiovascular disease.
The finding that ESRD risk is higher than cardiovascular risk for African Americans with hypertensive nephrosclerosis is in direct contrast to what has been previously reported in other CKD populations. "The AASK trial and the subsequent cohort study allow the medical community to gain a broader understanding of incident cardiovascular disease and mortality during long-term follow-up in an entirely African-American population with nondiabetic hypertensive nephrosclerosis," comments Dr. Alves.
The findings are limited by the fact that the primary goal of the AASK trial was to detect changes in kidney function, ESRD, and/or risk of death. Cardiovascular events were measured as a secondary outcome.
The results may provide additional insight into the relationship between high blood pressure and kidney disease in African Americans, as well as some of the reported racial differences in the rates and outcomes of ESRD. "The study is timely given the increased recognition of medical health disparities observed among African American patients," Dr. Alves adds. "This type of information is needed if solutions are to be sought at the clinical and policy levels." ###
The AASK studies were sponsored by the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health.
The study abstract, "African-Americans (AA) with Hypertensive Nephrosclerosis Are Paradoxically More Likely To Reach End Stage Renal Disease (ESRD) Than Have a Cardiovascular Event," (TH-FC051) will be presented as part of a Free Communications session on the topic of "Effects of Traditional and Nontraditional Risk Factors on Cardiovascular Risk in Chronic Kidney Disease and End Stage Renal Disease" on Thursday, November 6, at 5:36 p.m. in Room 108 of the Pennsylvania Convention Center in Philadelphia, PA.
ASN is a not-for-profit organization of 11,000 physicians and scientists dedicated to the study of nephrology and committed to providing a forum for the promulgation of information regarding the latest research and clinical findings on kidney disease. ASN Renal Week 2008, the largest nephrology meeting of its kind, will provide a forum for 11,000 nephrologists to discuss the latest findings in renal research and engage in educational sessions related to advances in the care of patients with kidney and related disorders. Renal Week 2008 will take place November 4 – November 9 at the Pennsylvania Convention Center in Philadelphia, PA.
Contact: Shari Leventhal sleventhal@asn-online.org WEB: American Society of Nephrology
Saturday, November 8, 2008
Family problems affect African-American children more than other races
Stephen M. Gavazzi of The Ohio State University, Jennifer M. Bostic and Courtney M. Yarcheck of the OSU Center for Family Research, and Ji-Young Lim of Miami University of Ohio examined factors related to gender, race/ethnicity, family factors, and mental health issues is a sample of 2,549 Caucasian and African American youth coming to the attention of juvenile courts. ###
This study is published in the Journal of Marital and Family Therapy. Media wishing to receive a PDF of this article may contact journalnews@bos.blackwellpublishing.net.
Stephen Gavazzi is affiliated with The Ohio State University and can be reached for questions at gavazzi.1@osu.edu.
The Journal of Marital & Family Therapy (JMFT) is published quarterly by the American Association for Marriage and Family Therapy (AAMFT) and, with over 20,000 subscribers, is the best known and most influential family therapy journal in the world.
Wiley-Blackwell was formed in February 2007 as a result of the acquisition of Blackwell Publishing Ltd. by John Wiley & Sons, Inc., and its merger with Wiley's Scientific, Technical, and Medical business. Together, the companies have created a global publishing business with deep strength in every major academic and professional field. Wiley-Blackwell publishes approximately 1,400 scholarly peer-reviewed journals and an extensive collection of books with global appeal. For more information on Wiley-Blackwell, please visit www.wiley-blackwell.com or interscience.wiley.com.
Contact: Amy Molnar journalnews@bos.blackwellpublishing.net 201-748-8844 Wiley-Blackwell
Thursday, November 6, 2008
Minority patients discouraged from cancer screening by negative messages
 Robert A. Nicholson, PhD, Secondary Faculty, Department of Community Health, Division of Behavioral Science and Health Education. Donco Building Room # 208, Saint Louis University Medical Center. Tel:(314) 977-8490 nicholra@slu.edu WEB: Nicholson | Behavioral Science | PHILADELPHIA – New behavioral science research published in Cancer Epidemiology, Biomarkers & Prevention, a journal of the American Association for Cancer Research, found that constantly emphasizing the negative consequences of a lack of cancer screening among minorities can actually make them less likely to go for screening. "We have typically assumed that one of the best ways to motivate individuals is to point out disparities in health, but we may be having negative unintended consequences," said Robert Nicholson, Ph.D., an assistant professor in the Department of Neurology and Psychiatry at the St. Louis University School of Public Health. "Instead of motivating people who would be less likely to get these services in the first place, we may be driving them away." |
Nicholson and colleagues conducted a double-blind, randomized trial among 300 African-American adults. The adults were asked to read one of four articles about colon cancer and then answer questions about their likelihood of getting screened.
The first article emphasized that colon cancer was an important problem for African-Americans. The second emphasized that outcomes for blacks with colon cancer were worse than for whites, while a third said that although outcomes for African-Americans were improving the improvement was less than seen among whites. Finally, a fourth article discussed how outcomes for blacks with colon cancer were improving over time.
If African-Americans read the article that said outcomes for blacks were improving over time, they were more likely to have a positive emotional response than if they read any of the other three articles. The article most likely to cause a negative response was the one that simply stated the problem.
Similarly, those that read the article about African-Americans making progress in outcomes for colon cancer were far more likely to want to be screened than those who read any of the other three articles.
The mean age of the participants was 54.4 years, 76 percent were women and 89 percent had completed high school. Comprehension analysis found that all participants understood what they had read.
Nicholson said they did not ask questions about motivation, but he suggests that a general mistrust of the medical community may be playing a role. If information reinforces that mistrust, then African-Americans are less likely to be screened.
"We believe that a positive message would go a long way toward overcoming mistrust," Nicholson said. "We need the right kind of message for the right kind of person, and not to assume that what we have always done is working." ###
The mission of the American Association for Cancer Research is to prevent and cure cancer. Founded in 1907, AACR is the world's oldest and largest professional organization dedicated to advancing cancer research. The membership includes more than 28,000 basic, translational and clinical researchers; health care professionals; and cancer survivors and advocates in the United States and 80 other countries.
AACR marshals the full spectrum of expertise from the cancer community to accelerate progress in the prevention, diagnosis and treatment of cancer through high-quality scientific and educational programs. It funds innovative, meritorious research grants. The AACR Annual Meeting attracts more than 17,000 participants who share the latest discoveries and developments in the field. Special conferences throughout the year present novel data across a wide variety of topics in cancer research, treatment and patient care.
AACR publishes five major peer-reviewed journals: Cancer Research; Clinical Cancer Research; Molecular Cancer Therapeutics; Molecular Cancer Research; and Cancer Epidemiology, Biomarkers & Prevention. The AACR's most recent publication and its sixth major journal, Cancer Prevention Research, is dedicated exclusively to cancer prevention, from preclinical research to clinical trials. The AACR also publishes CR, a magazine for cancer survivors and their families, patient advocates, physicians and scientists. CR provides a forum for sharing essential, evidence-based information and perspectives on progress in cancer research, survivorship and advocacy.
Contact: Jeremy Moore Jeremy.moore@aacr.org 267-646-0557 American Association for Cancer Research
Tuesday, November 4, 2008
African-Americans have unique lung cancer risks from chronic obstructive pulmonary disease
What was unique to African Americans was the risk associated with chronic obstructive pulmonary disease. African American men with a prior history of chronic obstructive pulmonary disease had a more than sixfold increased risk of lung cancer, similar to that seen with smoking. This is approximately two-fold higher than the risk typically seen from chronic obstructive pulmonary disease among whites.
"The one size fits all risk prediction clearly does not work," said Carol Etzel, Ph.D., assistant professor of epidemiology at the University of Texas M.D. Anderson Cancer Center.
As with whites, smoking was a significant risk factor for lung cancer. Current smokers had a more than sixfold increased risk of lung cancer, and former smokers had a more than threefold increased risk. This decreased risk was confined to those who had quit smoking more than ten years prior to diagnosis; these patients had a 58 percent decreased risk compared with patients who had quit within the previous ten years.
Researchers also found that hay fever, previously shown to be protective among whites, was also protective among African Americans. Specifically, African Americans with hay fever were 44 percent less likely to develop lung cancer, a rate that had been previously seen among whites.
African American males have a higher risk of lung cancer incidence at 110.6 per 100,000 compared with 81 per 100,000 among white males. Mortality is also higher among African American men at 95.8 per 100,000 compared with 72.6 among whites. Lung cancer incidence and mortality rates among women are comparable.
Etzel said the risk prediction model detailed in Cancer Prevention Research is part of an ongoing project to establish risk models among different ethnic groups; a model for Hispanics is currently under development.
"What we hope is that a doctor can use these models to encourage their patients to take steps to prevent lung cancer. Even if they are never smokers, they can be at risk," said Etzel. ###
The mission of the American Association for Cancer Research is to prevent and cure cancer. Founded in 1907, AACR is the world's oldest and largest professional organization dedicated to advancing cancer research. The membership includes more than 28,000 basic, translational and clinical researchers; health care professionals; and cancer survivors and advocates in the United States and 80 other countries.
AACR marshals the full spectrum of expertise from the cancer community to accelerate progress in the prevention, diagnosis and treatment of cancer through high-quality scientific and educational programs. It funds innovative, meritorious research grants. The AACR Annual Meeting attracts more than 17,000 participants who share the latest discoveries and developments in the field. Special conferences throughout the year present novel data across a wide variety of topics in cancer research, treatment and patient care.
AACR publishes five major peer-reviewed journals: Cancer Research; Clinical Cancer Research; Molecular Cancer Therapeutics; Molecular Cancer Research; and Cancer Epidemiology, Biomarkers & Prevention. Its most recent publication and its sixth major journal, Cancer Prevention Research, is dedicated exclusively to cancer prevention, from preclinical research to clinical trials. The AACR also publishes CR, a magazine for cancer survivors and their families, patient advocates, physicians and scientists. CR provides a forum for sharing essential, evidence-based information and perspectives on progress in cancer research, survivorship and advocacy.
Contact: Jeremy Moore Jeremy.moore@aacr.org 267-646-0557 American Association for Cancer Research
Sunday, November 2, 2008
MYH9 gene variations help explain high rate of kidney disease in African-Americans
Several recent studies have suggested that common gene variations may be responsible for much of the elevated risk of kidney disease in African Americans. New research on the MYH9 gene—and its implications for the screening and possible prevention of kidney disease in the African American population—will be summarized in a press briefing to be held at the American Society of Nephrology's 41st Annual Meeting and Scientific Exposition in Philadelphia, PA.
"The susceptible variants in the gene MYH9 are very frequent among African Americans and account for a substantial proportion of the higher risk of end-stage renal disease (ESRD) in African Americans compared to European Americans," comments Rulan S. Parekh, MD, of Johns Hopkins University School of Medicine in Baltimore, MD, who will introduce the press briefing. "Discovery of this gene has opened up a new area of research to focus on both the mechanism of disease and also potential use for screening in the population."
In September, researchers from the National Institutes of Health (NIH) in Bethesda, MD, and Johns Hopkins University published independent studies showing that variations of the "non-muscle myosin heavy chain 9" gene (MYH9) are linked to certain types of kidney disease that are more common in African Americans, including focal segmental glomerulosclerosis (FSGS), HIV-associated nephropathy, and non-diabetic ESRD.
Variations of MYH9 may also explain the increased rate of hypertension-related kidney disease in African Americans, which tends to persist even with effective treatment to lower blood pressure. Overall, the gene variants appear to increase the risk of developing any form of ESRD, which is irreversible kidney failure requiring dialysis or transplantation not related to diabetes.
The discoveries have major public health implications because of the high frequency of MYH9 variants among African Americans with kidney disease: up to 60 percent, compared with four percent of European Americans.
At the press briefing, Dr. Parekh will introduce a panel of researchers at the forefront of ongoing research on MYH9. The speakers will share their perspectives on the discoveries so far, key areas for further study, and the implications for risk screening and efforts to reduce kidney disease in the African-American population.
Cheryl Winkler, PhD, of NIH will summarize key findings on the link between MYH9 and FSGS, including the methods and concepts that led to the discoveries. New studies by Dr. Winkler, along with Jeffrey Kopp, MD, and other NIH researchers, suggest that MYH9 explains most of the racial difference in FSGS risk (F-FC254). Research by Dr. Kopp and Dr. Winkler will also be presented as part of a free communications session entitled, "Gene Mapping in Common Kidney Diseases" on Friday, November 7, from 4:00 p.m.-6:00 p.m. in Room 104 of the Pennsylvania Convention Center.
Dr. Winkler will also discuss new research on the geographic distribution of the MYH9 risk alleles (TH-PO107). Rates of highest-risk gene variant appear highest in populations from southern Africa; in contrast, the high-risk allele is infrequent in Europeans, and "rare to absent" in Asians. The findings suggest that selection of the high-risk MYH9 risk variants was an ancient event in human evolution (TH-PO109). Dr. Winkler will also present her research findings for poster numbers TH-PO107 and TH-PO109 on Thursday, November 6, from 10:00 a.m.-Noon in Hall A/B of the Pennsylvania Convention Center.
Linda Kao, PhD, of Johns Hopkins University will focus on the risk of non-diabetes-related ESRD related to MYH9 variants. Dr. Kao and Dr. Parekh were involved in the genome-wide study showing that the risk of nondiabetic ESRD is strongly related to higher African American ancestry on chromosome 22 (F-FC255). People with the MYH9 at-risk variants were at up to double the risk of having nondiabetic ESRD. In contrast, MYH9 does not affect the risk of ESRD resulting from diabetes, which remains the most common cause of kidney disease. Dr. Kao's research will also be presented as part of a free communications session entitled, "Gene Mapping in Common Kidney Diseases" on Friday, November 7, from 4:00 p.m.-6:00 p.m. in Room 104 of the Pennsylvania Convention Center.
Barry I. Freedman, MD, of Wake Forest University in Winston-Salem, NC, will discuss evidence on the relationship between MYH9 and early kidney disease. A new study suggests that these common MYH9 variants are related to albuminuria—leakage of the protein albumin in the urine, an early sign of kidney disease—in African Americans with high blood pressure, but not necessarily in European Americans (TH-PO108). Many cases of kidney disease attributed to hypertension or unknown causes in African Americans may actually be related to MYH9 variants, through a process similar to FSGS (TH-PO94). It's too early to tell whether MYH9 is related to lupus nephritis—another cause of kidney disease that's more common in African Americans (TH-PO106). On Thursday November 6, Dr. Freedman will also present his research on poster numbers TH-PO108, TH-PO94, and TH-PO106 from 10:00 a.m.-Noon in Hall A/B of the Pennsylvania Convention Center.
Dr Kopp will summarize the findings of the genetic risk associated with MYH9 variants and kidney disease. He will also address the implications of the new discoveries for patients and physicians, including the possible role of MYH9 screening.
The presentations will be followed by a brief question-and-answer session, moderated by Dr. Parekh. It's important to note that most African Americans with MYH9 gene variants will not develop kidney disease. However, MYH9 gene testing may become an important new tool to identify African American patients and families at increased risk. "In the future, therapeutics and screening may target those who have MYH9 genetic variants to prevent progression to ESRD," according to Dr. Parekh. ###
The Press Briefing, "Discovery of a Gene Associated with Kidney Diseases among African Americans," will be presented on Friday, November 7, 2008, from 12:15 p.m.-1:15 p.m. in Room 303A of the Pennsylvania Convention Center in Philadelphia, PA.
ASN is a not-for-profit organization of 11,000 physicians and scientists dedicated to the study of nephrology and committed to providing a forum for the promulgation of information regarding the latest research and clinical findings on kidney disease. ASN Renal Week 2008, the largest nephrology meeting of its kind, will provide a forum for 11,000 nephrologists to discuss the latest findings in renal research and engage in educational sessions related to advances in the care of patients with kidney and related disorders. Renal Week 2008 will take place November 4 – November 9 at the Pennsylvania Convention Center in Philadelphia, PA.
Contact: Shari Leventhal sleventhal@asn-online.org WEB: American Society of Nephrology
Image Licensing: Permission is granted to copy, distribute and/or modify this document under the terms of the GNU Free Documentation License, Version 1.2 or any later version published by the Free Software Foundation; with no Invariant Sections, no Front-Cover Texts, and no Back-Cover Texts.
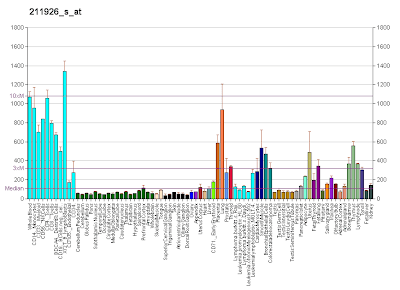
* Image Description: Gene expression pattern of the MYH9 gene.
* Image Source: Diagram created by User:AndrewGNF based on data from Su AI, Wiltshire T, Batalov S, et al (2004). "A gene atlas of the mouse and human protein-encoding transcriptomes". Proc. Natl. Acad. Sci. U.S.A. 101 (16): 6062–7. doi:10.1073/pnas.0400782101. PMID 15075390. Creation supported by the Genomics Institute of the Novartis Research Foundation.
Friday, October 31, 2008
Researchers Advance Health Communication for At-Risk Populations
 Glen Cameron Professor Strategic Communication Maxine Wilson Gregory Chair in Journalism Research. 140-E Walter Williams Hall, Missouri School of Journalism, Columbia, MO 65211-1200 Phone: 573-884-2607, Fax: 573-882-4823, E-mail: camerong@missouri.edu | The $8.6 Million Grant Will Fund Efforts to Improve Health Literacy, Health Outcomes. Columbia, Mo. -- The National Cancer Institute (NCI) has awarded an $8.6 million grant to the University of Missouri Health Communication Research Center (HCRC), in partnership with Washington University in St. Louis, to advance health communication that will improve health literacy and health outcomes for at-risk populations. The project promotes the importance of ensuring access to understandable health information. According to the National Assessment of Adult Literacy, only 12 percent of adults have proficient health literacy, which means that they have the skills needed to manage their health. The announcement supports Health Literacy Month, which is recognized in October. The renewal grant will fund the continuation of Ozioma (which means "good news" in Nigerian), a biweekly news service created by MU researchers that produces localized cancer-related news releases for black communities. |
The researchers analyzed the effectiveness of the news service and found that providing localized cancer news to black newspapers increased cancer news coverage and, therefore, prompted changes in readers' behaviors.
Our goal is to build on the findings from the Ozioma study by advancing tailored communication and health public relations to improve health outcomes for at-risk and general populations," said Jon Stemmle, HCRC assistant director. "We will develop a news information bureau that will provide locally relevant and race-specific cancer news stories to minority newspapers in predominately minority markets throughout the United States."
The news service will provide health stories to 36 newspapers. According to the researchers, the objective is to develop a permanent news service for NCI that targets every minority newspaper service in the United States.
"Providing people with understandable health information is essential to improving their health literacy," said Glen T. Cameron, HCRC director and the Maxine Wilson Gregory Chair in Journalism Research. "We hope to engage media in this process through our new news service, Informing Smart Health Decisions (I-SHD). Most press releases are general in form, created for the mass media audience. I-SHD is a cutting-edge approach to media relations that localizes a general release by region, state or community. We use local quotes, graphics and data to make the story more meaningful both for the local media and their audience."
The HCRC team consists of Cameron, Stemmle and María Len-Ríos, an assistant professor of strategic communication at the School, and a team of HCRC graduate students. The project also will include members of the Health Communication Research Laboratory at Washington University in St. Louis.
Contact: Emily Smith SmithEA@missouri.edu 573-882-3346 University of Missouri-Columbia
Wednesday, October 29, 2008
Teacher recruitment program will put more African-American men in Florida elementary schools
In Florida, where less than 1 percent of elementary teachers are black men, the program will be housed with the North East Florida Educational Consortium (NEFEC), and initially delivered at five community colleges, mostly in the northeastern part of the state. As the participants — the Misters — finish their first two years of school, they will transfer to three senior-level colleges taking part in Call Me MISTER: the University of Florida, the University of North Florida and Bethune-Cookman University.
The Misters are largely selected from under-served, socioeconomically disadvantaged and educationally at-risk communities. After graduation, they are expected to return to critical-need schools.
“I am elated about this program that addresses the shortage of minority males in the classroom. In my 11 years of recruiting teachers, particularly minorities, there has not been any initiative that empowers, encourages and excels like Call Me MISTER,” said Ulysees L. Gilbert II, coordinator of educator recruitment at NEFEC. “We are blessed to have this program in our state and many thanks to Rep. Joe Pickens — now the next president of St. Johns River Community College — for making it happen financially.”
Pickens arranged for a presentation to Gov. Charlie Crist’s chief of staff, which, with the cooperation of Education Commissioner Eric Smith, led to a one-year $300,000 appropriation for the program.
“I am thrilled at the opportunity to bring this program to Florida,” said Pickens. “I know firsthand that we don’t have enough black male teachers to be role models for a significant segment of our student population.”
As a former school board attorney, Pickens said he observed the shortage for many years.
Call Me MISTER’s director says the program has a proven track record for recruiting and training, and that original goal of doubling the numbers in South Carolina will be exceeded with the graduation of 100 Misters currently enrolled in the program.
“This is an excellent opportunity for the state of Florida and Call Me MISTER,” said Roy Jones, who oversees the program from his office at Clemson University. “Call Me MISTER in Florida will take things to a new level. It will become a national model for teacher recruitment.”
The first cohort of Misters in Florida will begin in January with 25, five each at St. Johns Community College in Palatka, the host college for the program; Florida Community College in Jacksonville; Lake City Community College; Central Florida Community College in Ocala; and North Florida Community College in Madison.
Call Me MISTER (Mentors Instructing Students Toward Effective Role Models) is licensed through Clemson University. License fees are reinvested into the management and further development of the program.
Call Me MISTER can be found in Georgia, Missouri, Pennsylvania and Virginia, in addition to South Carolina, where it is available to young men in 13 institutions of higher education across the state. An agreement for a program in Kentucky is pending.
END
CONTACT: Roy Jones, 864-656-7915 royj@clemson.edu CONTACT: Ulysses L. Gilbert, 386-329-3800 GilbertU@nefec.org WRITER: Ross Norton, 864-656-4810 rnorton@clemson.edu WEB: Clemson Home
Monday, October 27, 2008
Hypertension Disparity Linked to Environment
Social environment may play a greater role in the disparity between the numbers of African Americans living with hypertension compared to non-Hispanic whites with the disease. A study by researchers at the Johns Hopkins Bloomberg School of Public Health found that the disparity was substantially reduced when comparing groups of African Americans and non-Hispanic whites living in similar social environments. The results are published in the November 2008 print edition of Social Science and Medicine.
“Our study found that nearly 31 percent of the hypertension disparity among African Americans and non-Hispanic whites is attributable to environmental factors,” says Roland James Thorpe Jr., PhD, lead author of the study and an assistant scientist with the Bloomberg School’s Hopkins Center for Health Disparities Solutions. “These findings show that ethnic disparities could be linked to a number of factors other than race. Careful review of psychosocial factors, stress, coping strategies, discrimination and other personality characteristics could play a large role in reducing or eliminating the disparity.”
Commonly referred to as the “silent killer,” hypertension is the most common cardiovascular disease, affecting 65 million adults in the U.S. Hypertension is a serious condition that can damage the heart and blood vessels and eventually lead to stroke, heart failure, heart attack, kidney failure and vision problems. Previous studies have found that African Americans tend to have an earlier onset and higher prevalence of the disease than non-Hispanic whites.
Thorpe, along with colleagues from the Bloomberg School’s Center for Health Disparities Solutions and North Carolina Central University, compared data from the Exploring Health Disparities in the Integrated Communities (EHDIC) study and the National Health and Nutrition Examinations Survey (NHANES) to determine if racial disparities in hypertension persisted in communities where there is a minimal difference in social environments. The EHDIC study examines racial disparities among African Americans and non-Hispanic whites with the same median socioeconomic status who reside in the same community. NHANES, a cross-sectional survey, reviews the health, function and nutritional status of people in U.S.
“After adjusting for demographic variables, our research found that while African Americans still displayed greater odds of being hypertensive compared to non-Hispanic whites, there was a dramatic decrease in the ratio. Our study concluded that race differences in social and environmental exposures partially accounted for race differences in hypertension,” said Thomas LaVeist, PhD, senior author of the study and director of the Hopkins Center for Health Disparities Solutions. “These findings support our theory that the disparity is likely caused by environmental factors along with several external factors and not biological differences among race groups, as previously suspected.”
“Social context as an explanation for race disparities in hypertension: Findings from the Exploring Health Disparities in Integrated Communities (EHDIC) Study” was written by Roland James Thorpe, Dwayne T. Brandon and Thomas A. LaVeist.
The researchers were funded by grants from the National Center on Minority Health; Health Disparities of the National Institutes of Health (NIH); and Pfizer, Inc.
Public Affairs media contact: Natalie Wood-Wright at 410-614-6029 or nwoodwri@jhsph.edu.
Contact: Natalie Wood-Wright nwoodwri@jhsph.edu 410-614-6029 Johns Hopkins University Bloomberg School of Public Health
Saturday, October 25, 2008
Making a difference in minority health
Nurses and Barbers Work Together to Promote Prostate Cancer Prevention
Prostate cancer is the second-leading cause of death in African-American men, higher than any other racial or ethnic group. To create an opportunity for African-American men to learn about prostate cancer prevention in their own communities, CMH developed Health Advocates In Reach (HAIR). HAIR trains barbers to deliver accurate health information to peers and customers with the assistance of oncology nurses, public health professionals and prostate cancer survivors. Since 2005, CMH project director Mario Browne, M.P.H., has coordinated the efforts of HAIR, which has reached 275 men with prostate cancer information and screened 139 African-American men.
Abstract number 186259, scheduled for 8:30 a.m. PDT, Monday, Oct. 27
The Underground Railroad Bicycle Route: Exploring African-American History by Bicycle
To increase physical activity among African-Americans and diversify the cycling community, CMH partnered with Adventure Cycling Association in 2004 to create the Underground Railroad Bicycle Route, a 2,100 mile cycling route from Mobile, Ala. to Owen Sound, Ontario. In May 2007, 20 riders from across the U.S. launched the inaugural tour, spanning 53 days. Since that time, organizers have developed two maps for the route – a long distance and short distance tour to accommodate all types of cyclists. Led by the director of CMH, Stephen Thomas, Ph.D., Philip Hallen Professor of Community Health and Social Justice, and Mario Browne, M.P.H., CMH project director, the project combines history, culture and education to celebrate the courage and determination of freedom seekers and to engage people of all walks of life in physical activity. Hundreds of cyclists of all races, ethnicities and ages have cycled all or portions of the bike route since 2007.
Abstract number 181775, scheduled for 3:12 p.m. PDT, Monday, Oct. 27 ###
CMH was established in 1994 with a grant from the Richard King Mellon Foundation. CMH is committed to taking a lead role in the nation's prevention agenda to eliminate racial and ethnic health disparities as described in Healthy People 2010, a Department of Health and Human Services Initiative. For more information on CMH, visit http://www.cmh.pitt.edu.
Contact: Clare Collins collcx@upmc.edu 412-352-2886 University of Pittsburgh Schools of the Health Sciences
Wednesday, October 22, 2008
Race and insurance status associated with death from trauma
Adil H. Haider, M.D., M.P.H., of the Johns Hopkins University School of Medicine, Baltimore, and colleagues reviewed data from the National Trauma Data Bank for 429,751 patients age 18 to 64 years treated at approximately 700 trauma centers nationwide between 2001 and 2005. Of these, 72,249 were African American, 41,770 were Hispanic and 262,878 were white; 47 percent had health insurance.
Overall, death rates were higher among African American (8.2 percent) and Hispanic (9.1 percent) patients than among white patients (5.7 percent). Uninsured patients were also more likely to die than insured patients (8.6 percent vs. 4.4 percent). "Mortality rates were substantially higher for all uninsured patients, almost doubling for African American (4.9 percent to 11.4 percent) and Hispanic patients (6.3 percent to 11.3 percent) compared with white patients (4.2 percent to 7.9 percent)," the authors write. "The absence of health insurance increased a trauma patient's adjusted odds of death by almost 50 percent."
Patients in minority groups were much more likely to be uninsured than white patients—about one-third of white patients, two-thirds of African American patients and two-thirds of Hispanic patients lacked insurance. Lack of insurance is associated with poorer baseline health status; because pre-existing conditions are known to affect trauma outcomes, this could partially account for the higher death rates in the uninsured, the authors note.
However, insurance status alone could not explain all racial disparities in trauma death rates. "Of the insured patients, both Hispanic and African American patients had significantly higher odds of mortality compared with white patients," the authors note. Other issues that may contribute to racial differences include mistrust, subconscious bias and stereotyping, but further study is needed to explore these possibilities, they continue.
"Understanding insurance and race-dependent differences is a crucial first step toward ameliorating health care disparities," the authors conclude. "The next step will be to comprehend the underlying reasons for these differences, which will enable the development of interventions to close the gap between patients of different races and payer statuses." ###
(Arch Surg. 2008;143[10]:945-949. Available pre-embargo to the media at www.jamamedia.org.)
Editor's Note: This study was supported by the Johns Hopkins University School of Medicine Department of Surgery New Faculty Academic Support Group. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
Contact: Eric A. Vohr evohr1@jhmi.edu 410-955-8665 JAMA and Archives Journals
Monday, October 20, 2008
Racial disparities in cardiovascular health linked to birth weight, slavery
Evanston, Ill. - October 16, 2008 – Two new articles examine the theory of "fetal programming" and their effect on racial health disparities. The studies, published in American Journal of Human Biology, suggest that the higher rates of hypertension and cardiovascular disease present in African Americans may be a consequence of low birth weights, and that these low birth weights may be a result of social rather than genetic factors.
It is well-established that the nutritional and psychological state of a pregnant mother can influence whether her child will later develop cardiovascular disease as an adult.
Nutrients and hormones present in the womb shape a fetus's development, in part by silencing certain genes in the body. These influences can persist into later life to impact adult health. Researchers from Northwestern University argue that such intergenerational impacts of environmental factors could help explain black-white differences in cardiovascular health in the U.S.
A second study in the Journal states that the average birth weight among African-American babies is approximately 250 grams lower than the average birth weight of whites, a difference that represents nearly 10 percent of an average infant's body weight. According to Grazyna Jasienska, co-author of the study, this may also be the result of conditions experienced by their ancestors during the period of slavery passed through epigenetic, rather than genetic, mechanisms.
Current socio-economic conditions which are, on average, worse for African-Americans, can explain only part of the observed birth weight variation, according to Jasienska. Nor is there reason to think that lower birth weight of African-Americans is due to original African genetic heritage. Prior studies have shown that contemporary black women who were born in African countries ancestral to slave populations, but who live in the U.S., give birth to children with significantly higher weight than black women in the U.S. who have slave ancestry.
"Slaves experienced poor nutrition during all stages of life, suffered from a heavy burden of infectious diseases and, in addition, experienced high energetic costs of hard physical labor," says Jasienska. "Even a short-term nutritional deprivation of pregnant women, when very severe, has been shown to have an intergenerational effect," says Jasienska. Dutch women exposed to famine as fetuses in mid- and late gestation have also been shown to have reduced birth weights, and the effect was detectable years later because birth weight of their children was also reduced.
The fetal programming concept suggests that physiology and metabolism, including growth and fat accumulation of the developing fetus, and, thus its birth weight, depend on intergenerational signal of environmental quality passed through generations of matrilinear ancestors.
A child's birth weight depends on the condition of his or her mother during pregnancy but also, recent research indicates, on the conditions the mother faced as a child and even as a fetus. As a result, a child's birth weight may be influenced by nutritional conditions of its grandmother and even great-grandmother. The resulting effects can be seen in both childhood and adulthood, and include a higher risk of hypertension, diabetes and cardiovascular disease.
Jasienska states that, in the U.S. , the condition of many slaves did not immediately improve after the abolition of slavery, so the causes are not as far removed in time from contemporary African Americans as it may seem. Census data from the year 1900 showed that African Americans continued to suffer higher mortality than whites from all major diseases except cancer. Even though several generations have passed since then, it may not have been enough time to eliminate the negative impact of slavery on the health of the contemporary African-American population. ###
Contact: Sean Wagner, swagner@wiley.com 781-388-8550 Wiley-Blackwell